Osteochondrosis is a chronic disease symptomatically expresses dystrophic disorders in joint cartilage. Most of the time, there is oteochondrosis of the spine, when changes in intervertebral discs and intervertebral joints occur. Depending on the location, cervical, thoracic and lumbar osteochondrosis are distinguished. Osteochondrosis is also often found, in which all parts of the spine suffer. The pathology requires consultation with a doctor and an integrated approach to treatment.

Description
Spine diseases, like other chronic diseases, are quickly "getting younger". If previously back and joint pain has bothered the elderly, today patients 18 to 30 are increasingly treating doctors.
Scientists consider a person's frankness a prerequisite for the development of this disease, osteochondrosis is also facilitated by a prolonged position. In addition, with age, joint cartilage loses thin elasticity and elasticity; Intervertebral discs lose moisture and shock absorption capacity become vulnerable in the time of physical effort.
Reasons
The causes of cervical osteochondrosis are in loads and affect the cervical region in different circumstances. Consequently, the muscles in the neck begin to decrease intensely, thus compensating this load as a result of spasm, as well as a violation of blood flow in this area.
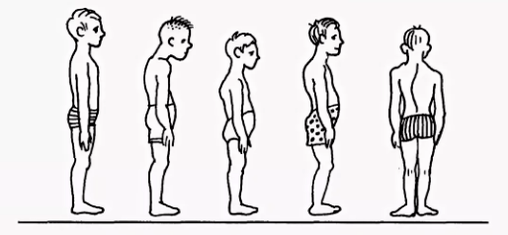
- In violation of posture scoliosis, balcony, round, kyphosis and other posture disorders, even if they are insignificant, cause a serious violation of the spine spine balance. As a result, the load on intervertebral discs is distributed unevenly, which causes its deformation and increased wear. The vertebrae begin to approach, causing violation of nerve processes, cervical osteochondrosis develops rapidly. Similar consequences have posture violations caused by a change in the natural position of the ribs.
- The muscle spasms spasmodic reactions of the back muscles, breast and press can lead to the fact that individual parts of the body are very tense. As a result, the overall position of body equilibrium is disturbed, causing a change in the position of the spine. Deformations may affect the cervical region region or other parts of the spine of the spine, causing osteochondrosis of the chest, cervical and lumbar parts.
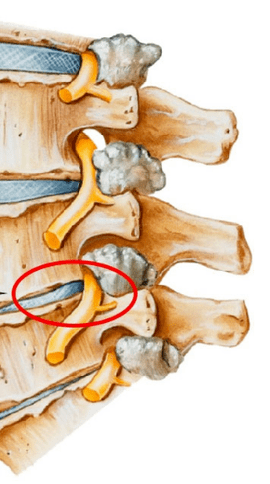
- In violation of blood supply, as vertebrates do not have a direct connection with the circulatory system, they receive nutrition from surrounding tissues. Infringement of blood supply to the cervical spine leads to the fact that the discs do not receive sufficient liquids for rehydration (the restoration of the form due to the absorption of moisture) and the renewal of the cartilage tissue. As a result, its wear is accelerated, there is a decrease in distances between the vertebrae of the cervical region, which leads to osteochondrosis.
- Injunction of innervation, a decrease in nerve root sensitivity leads to pathological changes in its structure, as a result of which the displacement and deformation of the cervical region vertebrae remain unnoticed by the patient. After all, pain is absent due to sensitivity disorders.
- Internal organs diseases are the wrong position of the internal organs, their displacement and lowering due to various dysfunctions lead to a violation of the general balance in the body. As a result, this sharply affects the position of the spine of the spine - the cervical, the lumbar vertebrae are displaced and deformed, leading to the corresponding types of osteochondrosis.
In general, cervical osteochondrosis develops due to the effects of adverse external factors that violate the natural equilibrium position of the spine and other human body systems.
Diagnosis
The diagnosis of cervical osteochondrosis begins with the collection of all the necessary information about the patient. The expert asks about the complaints that bother the person, are interested in their professional activities, as well as how they spend their weekend. An important point is the presence of osteochondrosis in parents, grandparents, because this is a disease of hereditary nature.
Then the doctor continues directly to the patient's visual examination. He studies the cervical compartment and his back to the curvature of posture, palpate the cervical region. This allows a specialist to evaluate the degree of development of the disease, because in advanced cases, the palpation of the cervical region causes marked pain.
When examining, you should pay attention:
- about the severity of cervical lordosis;
- shoulder height in the patient;
- the possibility of asymmetry of the supraclock areas;
- the possibility of neck asymmetry (for example, a consequence of congenital pathology or clear muscle spasm);
- The condition of the muscles of the shoulder waist and upper limbs (for example, an emitted muscle atrophy may indicate a compression of the cervical spine);
- The location of the chin - the chin is normal must be located along the middle line;
- Neck movement (flexion extortion, tilting the right and rotation and rotation).
Palpation is performed in the patient's starting position:
- lying on your back;
- lying in the stomach;
- Sitting in a chair.
The study of the volume of movements is also performed. It is performed in the patient's starting position sitting in a chair (to fix another column).
Distinguish the following basic movements in the cervical region:
- flexion;
- extension;
- lean to the right and left;
- Rotation.
About half of the volume of flexion and extension occurs between the back of the head, the vertebrae of C1 and C2. The rest of the movement is performed due to the underlying vertebrae, with a large scale of movements in C5-C7 vertebrae. Side inclinations are evenly distributed among all vertebrae.
To make an accurate diagnosis, additional studies are prescribed:
- X -ray of the cervical region. This method is appropriate in the early stages of the disease, but can be useless in advanced forms.
- CT (computed tomography). Allows you to see structural changes in the vertebrae, but with the help of this method, it is impossible to determine the size of the hernia between the vertebrae.
- Magnetic resonance imaging. It is considered the most effective method for diagnosing cervical osteochondrosis. You can determine the size of the hernia between the discs as well as the degree of their development.
- The doctor can also prescribe a duplex scan that allows us to determine a violation of normal blood circulation in the arteries.
Treatment
Treatment of cervical osteochondrosis is a complex therapy that includes taking medications, gels and various physiotherapeutic measures. An important role is played by therapeutic gymnastics as well as massage of the problem area.
Medicine
It is impossible to eliminate the consequences of degenerative-distribution changes in the spine without the use of medicines. The use of medicines in the treatment of cervical osteochondrosis is one of the main points of the complex approach of healing, used by most specialists in traditional medicine.
It is designed to solve multiple problems, including:
- Stop the symptom of pain and eliminate the inflammatory process;
- Remove muscle spasm;
- stimulate the process of regeneration of cartilage cells and bone tissue;
- Strengthen the protective properties of the body, increase immunity;
- Improve the general condition, eliminating other symptoms that interfere with recovery.
Depending on these purposes, all medications prescribed by a doctor suffering from cervical osteochondrosis can be conditionally divided into the following groups:
- Analgesics (non -esteroids that relieve pain).
- Anti -inflammatory (steroid) are hormonal drugs that relieve inflammatory phenomena and thus eliminating pain.
- CondoProtectors are medications containing substances that replace the components of cartilage tissue - chondroitin, hyaluronic acid.
- Muslaxantes. These are drugs that relax muscle tone. They are used in surgery and orthopedics as auxiliary remedies to interrupt pain. Such medications are administered by the parent and therefore always under the supervision of a doctor.
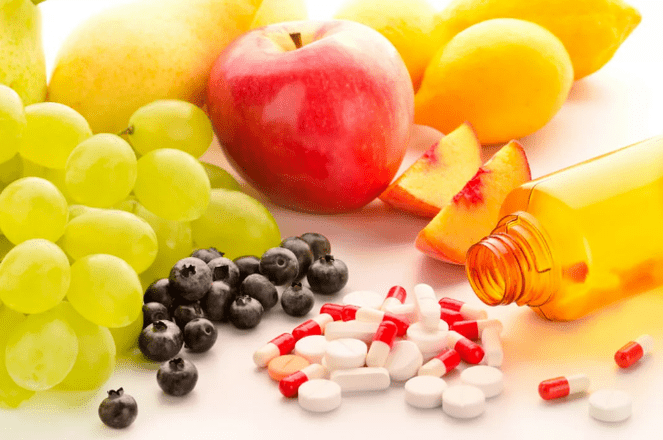
- Vitamins. With cervical osteochondrosis, vitamins are prescribed, beneficially affecting the peripheral nervous system and improving conductivity. Water -soluble vitamins: B1, B6, B12, Fat -soluble vitamins: A, C, D, E. In recent years, combined drugs containing painkillers and more frequently vitamin components.
- Ointments and gels for external use.
Physiotherapeutic
The main objective of physiotherapeutic treatment is to stimulate the body regeneration process and eliminate pain. The most popular methods in the treatment of cervical chondrosis are as follows:
- Ultrasound. The physical with ultrasound waves is used to relieve severe manifestations of pain and inflammatory reaction. Ultrasound is to massage neck tissue, after which metabolism is activated.
- Vibration massage. The impact on the pain area during vibration massage is through mechanical oscillatory movements. For the proper conduct of this physical therapy, a strip vibrorator is usually used.
- Electrophoresis. This method of conduction of physiotherapeutic care for cervical osteochondrosis is performed using diabnamic and modulated currents, as well as electric fields when the body is administered in the tissues of medicines. Electrophoresis perfectly relieves spasmodic syndromes and eliminates pain in the inflamed muscles.
- Magnetotherapy. The essence of magnetotherapy as physicalization in cervical region osteochondrosis is explained by the use of field constants or variables with a magnet, a frequency of different sizes. This method can help the patient remove pain and stop the inflammatory process in the fireplace. The procedure is often performed at home after the acquisition of a special magnetography device.
- Dutoenzor-therapy. Currently, a very popular physiotherapy method, consisting of stretching the spine of the spine under the mass of the patient's body. To perform this procedure, a special way is required, which has sloping ribs and they change the place under the weight of their own body. Muscle tone is normalized, which leads to relaxation.
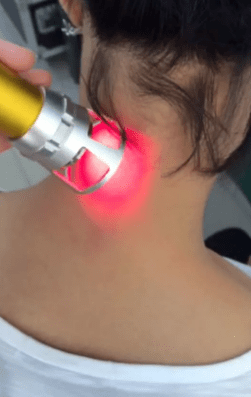
- Laser therapy. The laser has a complex effect on the focus of inflammation, activates biological processes in nervous system tissues. This allows you to get a positive effect of treatment. A complex effect on the body consists of the anti -inflammatory, analgesic and wound healing effect. A laser treatment procedure should not exceed 15 minutes. This is the ideal time of sector exposure of the Helic-Neon laser in the affected areas. In this case, laser duration in a pain should not exceed 2 minutes.
- Balneotherapy. The benefits of mineral water have been known for a long time, this is what Balneotherapy is based. The procedure implies the active use of water resources in the treatment of osteochondrosis. In addition to the adoption of baths, different types of souls and active swimming in the pool, therapy involves the use of therapeutic mud applications in painful areas of the body. The therapeutic effect is achieved by the simultaneous effect of chemically active substances contained in water under various temperature conditions. The technique allows you to interrupt pain syndrome, improving local microcirculation in tissues.
Exercise therapy
It should be remembered that exercise therapy is not performed when signs of exacerbation begin: pain. After the LFK complex, they can intensify and cause inconvenience.
There are several general recommendations for collection:
- Physical education should occur in closed environments with good ventilation, an excellent option on the street.
- Classes are performed only during the period of disease remission (when there are no symptoms).
- Clothing in exercise therapy should be wide, not embarrassing movements and breathing.
- All movements are soft, amplitude and the number of repetitions increase gradually.
- If the pain begins, you should immediately stop the lesson.
- Preced the classes and end pressure and pulse measurements. When these indicators differ from normal, the load should be reduced.
- It is advisable to hear your breathing throughout the lesson, this will increase efficiency. All stretching exercises are performed on expiration.
- It is very important to gradually increase the load and the number of repetitions, this will reduce the risk of injury and prevent overwork.
- Exercises are important to run regularly so you can get a quick result.
- Before starting independent classes, you need to consult a doctor and agree with him a set of exercises.

Recommended exercises in the starting position lying on the stomach:
- The head is at the end on the forehead, hands on the back of the head, elbows parallel to the floor. Raise your head with your hands, keep this position to 4 accounts, lower and relax. Repeat 2-4 times.
- The head is in the stop on the chin, palm trees under the chin. Time in time, stretch your arms forward, two - scattered to the sides, three - stretch forward, four - the starting position. Repeat 2-4 times.
- The hands stretched forward. Nothing the "rabbit" style, repeated 4-8 times.
- Palms under the chin, emphasis on the palm of your forehead. Alternatively, taking the heel from the buttocks. Repeat 4-8 times.
Recommended exercises in the starting position lying sideways (right, then left):
- The right hand is extended, the right ear is in it, lift the right hand with your head, keep the position to 4 accounts, lower and relax. Repeat 2-4 times.
- The left hand rests on the floor in front of the chest, the left leg causes the fly movements forward and backwards. Repeat 6-8 times.
- The left hand along the body, lift the left hand up and out, lower, lower. Repeat 2-4 times.
- The left hand in the thigh. Pulling both knees in the chest in the expiration, straightening the inspirational legs. Repeat exercises 2-4 times.

























